Our Services
We specialize in colon cancer screening, as well as, in the diagnosis and treatment of esophageal and gastric disorders, acid reflux, heartburn, dysphagia, small and large intestinal disorders, diarrhea, constipation, IBS, Celiac disease, Crohn’s and colitis.

 We provide a comprehensive evaluation to determine accurate diagnosis and develop appropriate treatment plans.
We provide a comprehensive evaluation to determine accurate diagnosis and develop appropriate treatment plans.
The right diagnosis is the first step in successfully treating digestive problems. During the consultation, we will obtain detailed information from you regarding your symptoms and medical history, followed by an appropriate physical exam, and then conclude by discussing with you our thoughts, impression, and recommendations. We utilize a wide array of tools for diagnosing GI problems including upper GI endoscopy, colonoscopy, radiological and laboratory studies, wireless capsule endoscopy, manometry, and breath testing. We work with various tertiary centers, and refer patients when necessary to GI experts when more advanced care is needed.
We offer a wide variety of appointment dates and times to ensure that our patients find an appropriate time that is convenient and compatible with their schedule. We strive to create an efficient and responsive consultation for every patient that visits our office.
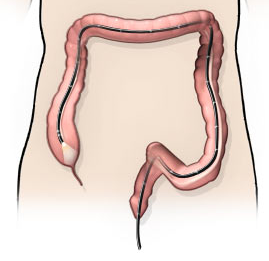 A colonoscopy is a procedure used to view the large intestine (colon and rectum) using an instrument called a colonoscope, a flexible tube with a small camera and light source attached to its tip. A colonoscopy can be performed for screening purposes for the detection of colon cancer, and for the prevention of colon cancer by detecting and removing polyps. Colonoscopy can also be performed to diagnose and monitor other disorders of the colon such as ulcerative colitis and Crohn’s disease.
A colonoscopy is a procedure used to view the large intestine (colon and rectum) using an instrument called a colonoscope, a flexible tube with a small camera and light source attached to its tip. A colonoscopy can be performed for screening purposes for the detection of colon cancer, and for the prevention of colon cancer by detecting and removing polyps. Colonoscopy can also be performed to diagnose and monitor other disorders of the colon such as ulcerative colitis and Crohn’s disease.
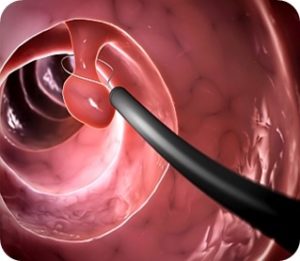
Colonoscopy is usually performed under sedation on an outpatient basis. You will be given laxatives to clear your bowels before the procedure. The colonoscope is inserted into the rectum and gently moved up the colon until it reaches the cecum (junction of small and large intestine). The colonoscope is then slowly withdrawn while carefully visualizing the colon on a screen. Any polyps or growths detected by the colonoscope can be removed and sent to the lab for determining whether it is cancerous or not. Biopsies can also be obtained during the colonoscopy for detecting microscopic abnormalities. Although rare, risks of a colonoscopy include perforation, bleeding, misdiagnosis, and complications of anesthesia.
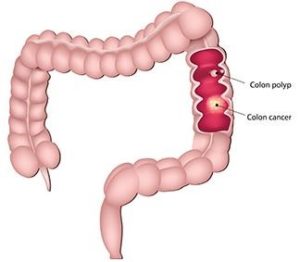 Colorectal cancer is one of the most common preventable cancers. A screening colonoscopy is the procedure of looking for polyps (noncancerous growths) and cancer in the rectum and colon. Some polyps can become cancerous. Polyps can be removed during a colonoscopy which helps prevents colon cancer. Polyps and early colon cancer often present without symptoms.
Colorectal cancer is one of the most common preventable cancers. A screening colonoscopy is the procedure of looking for polyps (noncancerous growths) and cancer in the rectum and colon. Some polyps can become cancerous. Polyps can be removed during a colonoscopy which helps prevents colon cancer. Polyps and early colon cancer often present without symptoms.
The people at high risk of colon cancer are:
- People above the age of 50
- People who have a history of colon cancer
- People whose close family members such as parents, siblings, or children have or had colon cancer
- People with ulcerative colitis or Crohn’s disease
- People with inherited familial adenomatous polyposis, a condition where individual develop number of polyps in the colon and rectum
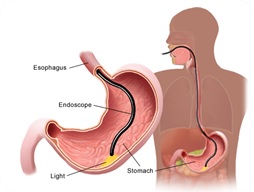 An upper GI endoscopy, also known as an esophagogastroduodenoscopy (EGD), is a procedure that enables your physician to examine the lining of the upper GI tract that includes the esophagus, stomach, and beginning of the small intestine (duodenum). An upper GI endoscopy is typically done to diagnose and treat conditions of the upper GI tract such as difficulty swallowing, abdominal pain, nausea, vomiting, or GI bleeding.
An upper GI endoscopy, also known as an esophagogastroduodenoscopy (EGD), is a procedure that enables your physician to examine the lining of the upper GI tract that includes the esophagus, stomach, and beginning of the small intestine (duodenum). An upper GI endoscopy is typically done to diagnose and treat conditions of the upper GI tract such as difficulty swallowing, abdominal pain, nausea, vomiting, or GI bleeding.
The instrument used in the upper GI endoscopy is known as an endoscope. It is a flexible tube about the thickness of a pencil. There is a light source and camera on the end of the endoscope; the image is projected into a video screen. While the patient is sedated, the endoscope is carefully inserted into the mouth and advanced to the duodenum. Biopsies (tissue samples) can be obtained and treatment of active bleeding can be done during the procedure. Esophageal dilation can also be performed during the procedure if there are narrow areas in your esophagus that are causing swallowing difficulty. An upper GI endoscopy takes about 10 minutes. Although rare, risks of an upper GI endoscopy include perforation, bleeding, misdiagnosis, and complications of anesthesia.
 Capsule Endoscopy is a diagnostic tool helpful in taking pictures of the digestive tract including esophagus, stomach and especially the small intestine. Small intestine is a difficult area to reach through conventional endoscopy and other imaging tests as it lies between the stomach and large intestine. In video capsule endoscopy, the patient swallows a capsule the size of a large vitamin pill. The capsule has a smooth coating making it easier to swallow. This capsule contains a camera, a bulb, battery and a transmitter. The camera takes thousands of pictures of the digestive tract during its passage through the digestive tract and transmits it to a recorder worn as a belt on the waist for about 12 hours to store the images. These images are transferred to a computer, and then converted into a video. The capsule is passed out of the body with stool and can be flushed away.
Capsule Endoscopy is a diagnostic tool helpful in taking pictures of the digestive tract including esophagus, stomach and especially the small intestine. Small intestine is a difficult area to reach through conventional endoscopy and other imaging tests as it lies between the stomach and large intestine. In video capsule endoscopy, the patient swallows a capsule the size of a large vitamin pill. The capsule has a smooth coating making it easier to swallow. This capsule contains a camera, a bulb, battery and a transmitter. The camera takes thousands of pictures of the digestive tract during its passage through the digestive tract and transmits it to a recorder worn as a belt on the waist for about 12 hours to store the images. These images are transferred to a computer, and then converted into a video. The capsule is passed out of the body with stool and can be flushed away.
The common diseases of the small intestine that are diagnosed through capsule endoscopy are:
- Gastrointestinal bleeding
- Tumors in the small intestine
- Crohn’s disease
- Celiac disease
- Polyps of the small intestine
Risks
Small bowel capsule endoscopy is a noninvasive and safe procedure. A rare risk associated with a capsule endoscopy is that the capsule can get stuck in the digestive tract. This is not a serious risk. The doctor will wait for some more time for it to come out on its own, but if it causes a bowel obstruction, it is taken out through conventional endoscopy or surgery as the last resort.
 Anorectal manometry is a test performed to evaluate patients with constipation or fecal incontinence. This test measures the pressures of the anal sphincter muscles, the sensation in the rectum, and the neural reflexes that are needed for normal bowel movements.
Anorectal manometry is a test performed to evaluate patients with constipation or fecal incontinence. This test measures the pressures of the anal sphincter muscles, the sensation in the rectum, and the neural reflexes that are needed for normal bowel movements.
The test takes approximately 30 minutes and is performed by a trained technician. The technician or nurse will explain the procedure to you and answer any questions you may have. The patient then lies on the left side. A small, thin (thinner than a pencil) flexible tube with a balloon at the end is inserted into the rectum. The catheter is connected to a computer that measures the pressures. During the test, the small balloon attached to the catheter may be inflated with air in the rectum to assess the normal reflex pathways. The technician will also ask the patient to squeeze, relax, and push at various times. The anal sphincter muscle pressures are measured during each of these maneuvers. To squeeze, the patient tightens the sphincter muscles as if trying to prevent anything from coming out. To push or bear down, the patient strains down as if trying to have a bowel movement. Lastly, the patient will be asked to cough a few times while the catheter measure anal sphincter pressure. After the test, you may drive yourself home and go about your normal activities.
 A lactose hydrogen breath test is used to diagnose lactose intolerance. Lactose intolerance causes symptoms such as diarrhea and bloating. After drinking a solution of lactose in water, you will be asked to breathe into a small device. Your breath samples will be analyzed for hydrogen or methane content to determine if you are properly breaking down the lactose. This test takes approximately 2 hours and is performed in our office in Dover, Delaware.
A lactose hydrogen breath test is used to diagnose lactose intolerance. Lactose intolerance causes symptoms such as diarrhea and bloating. After drinking a solution of lactose in water, you will be asked to breathe into a small device. Your breath samples will be analyzed for hydrogen or methane content to determine if you are properly breaking down the lactose. This test takes approximately 2 hours and is performed in our office in Dover, Delaware.
 A small bowel bacterial overgrowth test is used to diagnose small intestinal bacterial overgrowth, which causes GI symptoms such as diarrhea and bloating. After drinking a solution of glucose in water, you will be asked to breathe into a small device. Your breath samples will be analyzed for hydrogen or methane content to determine if you have small intestinal bacterial overgrowth. This test takes approximately 1 hour and is performed in our office in Dover, Delaware.
A small bowel bacterial overgrowth test is used to diagnose small intestinal bacterial overgrowth, which causes GI symptoms such as diarrhea and bloating. After drinking a solution of glucose in water, you will be asked to breathe into a small device. Your breath samples will be analyzed for hydrogen or methane content to determine if you have small intestinal bacterial overgrowth. This test takes approximately 1 hour and is performed in our office in Dover, Delaware.
 A fructose hydrogen breath test is used to diagnose fructose intolerance. Fructose intolerance causes symptoms such as diarrhea and bloating. After drinking a solution of fructose in water, you will be asked to breathe into a small device. Your breath samples will be analyzed for hydrogen or methane content to determine if you are properly breaking down the fructose. This test takes approximately 2 hours and is performed in our office in Dover, Delaware.
A fructose hydrogen breath test is used to diagnose fructose intolerance. Fructose intolerance causes symptoms such as diarrhea and bloating. After drinking a solution of fructose in water, you will be asked to breathe into a small device. Your breath samples will be analyzed for hydrogen or methane content to determine if you are properly breaking down the fructose. This test takes approximately 2 hours and is performed in our office in Dover, Delaware.
 A BreathTek test used to test for H. pylori (Helicobacter pylori), an infection caused by bacteria in your stomach. You will be asked to breath into a small collection bag. You will then be asked to drink a solution before breathing into a second bag. If your test shows you have H. pylori, you may be given a treatment of antibiotics.
A BreathTek test used to test for H. pylori (Helicobacter pylori), an infection caused by bacteria in your stomach. You will be asked to breath into a small collection bag. You will then be asked to drink a solution before breathing into a second bag. If your test shows you have H. pylori, you may be given a treatment of antibiotics.
